RESEARCH ARTICLE
An Overview on Polymethacrylate Polymers in Gastroretentive Dosage Forms
Pravin Gupta1, *, Manish Kumar2, Narsingh Sachan3
Article Information
Identifiers and Pagination:
Year: 2015Volume: 9
First Page: 31
Last Page: 42
Publisher Id: PHARMSCI-2-31
DOI: 10.2174/1874844901502010031
Article History:
Received Date: 30/12/2014Revision Received Date: 6/8/2015
Acceptance Date: 14/9/2015
Electronic publication date: 16/11/2015
Collection year: 2015
open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Drugs with lower bioavailability need repeated dosing to reach the minimum effective therapeutic concentration in plasma. In order to retain the drug in upper part of gastro intestinal tract (GIT) which is the major absorption window for majority of drugs and also to have localized effect many advances in drug delivery were made. Researchers mainly emphasize on to get patient compliance by formulating single dose, targeted and minimal side effects dosage form. The design must give constant drug release for longer time period that could be achieved through proper selection of polymers. These approaches in dosage design may also be advantageous for local action, to prevent drug degradation, delivery of gastro-irritant, narrow absorption window drugs and to get pH dependent release throughout the GIT. Polymethacrylate polymers in different ratios are available for the above objective as they are inert materials, could stay for longer time and are resistant to body fluids. This review also discusses the physicochemical properties of different available grades along with their glass transition temperatures (Tg).
1. INTRODUCTION
Drugs with shorter half-life get eliminated faster thus require frequent dosing. Attempts were made to release the drug slowly in the GIT so that a constant drug level could be maintained in the serum. Rapid gastric transit prevents complete drug release in the absorption zone and hence reduces the therapeutic efficacy of administered dose. Major challenges to improve the patient compliance includes: enabling the patient to self-administer, reduction in dosing frequency, ease of administration and to minimize the infections associated with the administration. To fulfill these requirements various drug delivery designs are developed. Gastro-retentive drug delivery system (GRDDS) tends to retain the dosage form in upper part of GIT through so many approaches. These systems have a bulk density less than that of gastric fluids and remain buoyant in the stomach without affecting the gastric emptying rate [1]. Retention of dosage form within the stomach depends on many factors mainly the density and size of the dosage form, the fasting and fed condition, the nature of the meal as well as posture of the patient [2].
Polymethacrylate polymers were used to entrap and encapsulate the drug so as to prevent its degradation in GIT. Various grades are commercially available and dissolve in specific pH region in GIT, which may be advantageous for the target drug delivery. They are prepared by free-radical polymerization technique. They are synthetic cationic, anionic or neutral polymers of dimethylaminoethyl methacrylates, methacrylic acid, and methacrylic acid esters in varying ratios. By varying the ratios of dimethylaminoethyl methacrylates, methacrylic acid, and methacrylic acid esters they are categorized as synthetic cationic, anionic or neutral polymers. Various commercially available polymers are in the form of dry powder, aqueous dispersion, or as organic solution [3]. They are mainly used as film formers in application for functional pharmaceutical coatings for controlling the release of drugs [4] and as matrix formers in granulation techniques [5]. Eudragit® acrylic resins are harmless and inert compounds, not absorbed in the GIT and are resistant to body fluids. They stay for a limited time in the GIT, are excreted unchanged, and do not produce degradation products [6]. Recent advances include the polymer microfabrication technology to produce particulate microstructure for drug delivery applications used for ocular, oral, transmucosal and injectable routes [7].
2. GASTRO RETENTIVE APPROACHES
Various approaches [8] are there for increasing the gastric-residence time (GRT) of the dosage forms (Fig. 1). Drug gets released at a desired rate from the system before emptied from the stomach and fluctuations in plasma drug concentrations could be avoided. Swelling and expanding dosage forms prevent their exit through the pylorus and help in retaining the entire dosage form. As these systems block the pyloric sphincter and hence referred to as plug type systems. Bio-adhesive systems utilize bio-adhesive polymers which adhere over the epithelial surface of the GIT and form mucous-polymer boundary through hydrogen and electrostatic bonding. They localize a delivery device within the lumen and cavity of the body enhancing the drug absorption in a site-specific manner. Modified shape systems have non-disintegrating geometric shapes which extend the GRT. High density formulations are made by coating the drug particles or granules with heavy inert materials like barium sulfate, zinc oxide, titanium dioxide, iron powder etc., [9] so their density becomes greater than the stomach contents and thus resist their exit.
List of available dosage form designs for gastric retention.
| Dosage form | Process | Raw materials | Characteristics of the product | Ref. no. |
|---|---|---|---|---|
| Ofloxacin-loaded pellets | Extrusion-spheronization | Ethyl cellulose, sodium bicarbonate, Eudragit RL 30D | Floats and retards the release over 8 h | [13] |
| Norfloxacin Microballoons | Emulsion solvent diffusion | Eudragit®L100, Eudragit®RS 100 | Intestinal pH dependent release | [14] |
| Bumetanide pellets | Fluid bed layering and coating | Eudragit®RS 100, Tri ethyl citrate, sodium chloride | Porous nature with sustained release | [15] |
| Levodopa novel unfolded CR-GRDF | Solvent evaporation | Gelatin, L-polylactic acid, ethyl cellulose, carbidopa, Eudragit®S 100 | Sustained drug release over 9 h | [16] |
| Novel floating effervescent | Ion exchange resins | Eudragit®RS 100 and sodium bi carbonate | Floated over 24 h | [17] |
| Diclofenac potassium pellets | Extrusion–spheronization | Eudragit®NE 30D, Eudragit®RS 30D and Kollicoat®SR 30D | Controls the release and fluctuations | [18] |
| Metformin hydrochloride matrix tablets | Direct compression | Polyethylene oxide and Eudragit®L100 | Unaffected by gastric pH | [19] |
| Levodopa floating coated mini-tabs | Melt granulation and compression | Eudragit®RL 30D, acetyl tri ethyl citrate | Buoyancy over 13 h and sustained release over 20 h | [20] |
| Riboflavin unfolding dosage form | Accordion pill technology | Eudragit® L and Eudragit® S plasticized with tri ethyl citrate | prolongs the gastric residence time | [21] |
| Diltiazem hydrochloride floating microspheres | Ionotropic gelation method | sodium alginate, calcium chloride, calcium carbonate, Eudragit®RS 30D and chitosan | Excellent floating ability with suitable drug release pattern over 24 h | [22] |
| Rabeprazole sodium enteric coated tablet | Wet granulation and direct compression | Colorcoat EC4S, Mannitol SD 200, microcrystalline cellulose and kollidon CL | Provides resistance to acidic environment and facilitates sustained release in alkaline conditions | [23] |
| Matrix tablet | Direct compression | Kollidon SR, Propanolol hydrochloride | Sustained the release over 24 h with fickian diffusion | [24] |
| Riboflavin microballoon | Emulsion solvent diffusion | Eudragit®RS 100 and hydroxyl propyl methyl cellulose | Urinary excretion was sustained | [25] |
| Ketoprofen floating microparticles | Emulsion solvent diffusion | Eudragit®S 100 and Eudragit®RL 100 | Gave higher percentage yield and better buoyancy | [26] |
| Riboflavin microballoons | Emulsion solvent diffusion | Eudragit®S 100, HPMC, PVA, dichloro methane and ethanol | Drug release from microballoons and total urinary excretion were strongly correlated | [27] |
| Verapamil floating pellets | Wet granulation and spheronization | Povidone K 30, Eudragit®NE 30 D, Eudragit®L 30 D, triethyl citrate, talcum | Floated for 6 h and gave improved pharmacokinetics than the conventional tablet | [28] |
| Microballoons | Emulsion solvent diffusion | Eudragit®S 100 and monostearin | Optimum temperature of 40 °C gave better buoyancy and retarded release due to smooth surface. Drug entrapment was high due to higher distribution coefficient | [29] |
| Riboflavin microballoons | Emulsion solvent diffusion | Eudragit®RS 100 and HPMC | Gamma scintigraphy technique confirms that the floating microballoons retained for longer time period in comparison to the non-floating in fed conditions, both half life and the total urinary excretion of drug increases significantly | [30] |
| Avidin microstructured Delivery | Microfabrication technology | Poly (methyl methacrylate) (PMMA) and Lectin | Adheres to the intestinal mucosa, prevents drug degradation and sustains the release | [32] |
 |
Fig. (1). Classification of gastroretentive drug delivery systems (GRDDS). |
For drugs locally absorbed through the stomach. e.g., ferrous salts and antacids, hydro dynamically balanced systems (HBS) are used. They proved to be useful for the administration of acidic substances like aspirin as it may cause irritation to the stomach wall. These systems result in complete dissolution of their content before empting the stomach so that the drug would be available for absorption in the small intestine without being affected by its alkaline pH. A short transit time as in case of diarrhea, poor absorption is expected so it may be advantageous to keep the drug in floating condition for relatively better response. Various limitations observed were: not suitable for drugs that have solubility or stability problems in GIT; high levels of fluid content are required for efficient float and dissolution; drugs with significant first pass metabolism are considered as the desired candidate suitable for gastric retention; some drugs even in the floating system may cause irritation to the gastric mucosa [10].
2.1. Suitable Drug Candidate
The drug candidate should have the appropriate properties like poor absorption in colonic region and better absorption in the upper part of GIT. So, the ideal drug candidates should have the following criteria [11]:
- Absorbed through upper part of GIT e.g., calcium supplement and cinnarazine.
- Drugs with narrow absorption window e.g., riboflavin and levodopa.
- Degrades in the colonic environment e.g., ranitidine HCl and metronidazole.
- Locally acting in the stomach e.g., antacids and misoprostol.
- Affecting the normal colonic bacteria e.g., amoxicillin tri hydrate.
- For eradication of helicobacter pylori responsible for chronic gastritis and peptic ulcer (tetracycline).
- Solubility problems at higher pH value e.g., Verapamil.
2.2. Suitable Polymers and Other Ingredients
- Polymers: Natural and synthetic polymers: HPMC K4 M, calcium alginate, Eudragit®S100, Eudragit®RL, Eudragit®RS, Eudragit®S, propylene foam, ethyl cellulose, methocel K4M, polyethylene oxide, β cyclodextrin, HPMC 4000, HPMC 100, CMC, polyethylene glycol, polycarbonate, PVA, sodium alginate, CP 934P, metolose SM 100, PVP, HPC, HPC L, HPC H, HPC M, HPMC, HPMC K4, polyox and carbopol etc.
- Inert fatty materials (5 %-75 %): Edible oils having specific gravity less than one can be used to decrease the hydrophilic property of the formulation and hence increase its buoyancy e.g. Beeswax, fatty acids, long chain fatty alcohols, Gelucires 39/01 and 43/01.
- Effervescent agents: Sodium bicarbonate, citric acid, tartaric acid, Di-SGC (Di-sodium glycine carbonate) and CG (citroglycine).
- Release rate accelerants (5 %-60 %): e.g. Lactose and mannitol.
- Release rate retardants (5 %-60 %): e.g. Di calcium phosphate, talc and magnesium stearate.
- Buoyancy increasing agents (up to 80 %): e.g. Ethyl cellulose.
- Low density material: e.g. Polypropylene foam powder (Accurel MP 1000) [12]
3. DESIGN AND FABRICATION
Gastro-retentive oral dosage form for controlled drug release could be governed by following principles [13]:
3.1. Dissolution Controlled Release
In oral dosage form the rate limiting step is dissolution and they are simplest to prepare. Drugs with slow dissolution rate are sustained of its own e.g., digoxin, griseofulvin and salicylamide. And for drugs with high dissolution rate can be sustained by coating the drug particles or granules with polymer solution or by making dispersion in polymer matrix. Dissolution control depends on thickness of the membrane barrier coat and on polymer core erosion. Most of the products fall in two categories:
3.1.1. Encapsulation Control
By coating of individual drug particles or granules by a slowly dissolving polymeric material, dissolution depends on the thickness and aqueous solubility of the polymers. In capsules the coated granules were fully dispersed in the GIT after 10-12 hrs whereas in tablets the release rate is affected by the influence of the excipients and compression.
3.1.2. Matrix Control
Drug is compressed with slowly dissolving carrier to form tablet. The rate of drug release depends on the rate of penetration of dissolution fluid to the matrix which in turn depends on the porosity, the presence of hydrophobic additives and the wettability and particle surface.
3.2. Diffusion Control
There are two types of diffusion controlled systems:
3.2.1. Reservoir Devices
Diffusion is controlled by water insoluble polymer; drug enters the membrane, diffuses to the periphery and is exchanged with the surrounding media. For constant release the polymer concentration is increased, that markedly increases the release rate of drug because the polymer leaches out rapidly from the system leaving large pores, so the solvent easily diffuses in to the polymer and facilitates drug release. Drug release from the insoluble polymer is inversely proportional to the film thickness and by increasing the hardness of the microcapsule the drug release rate can be prolonged.
3.2.2. Matrix Devices
Drug is dispersed in an insoluble matrix and the rate of drug release is dependent on diffusion and not on dissolution.
3.3. Diffusion and Dissolution Control
In this the dissolution of the polymeric membrane forms pores for the diffusion of drug particles through the polymer coat.
3.3.1. Ion-exchange Resins
They are water insoluble materials containing anionic or cationic groups in repeated positions in the chain. Release depends on the ionic environment of the resin, when high concentration of charged drug ions are in contact with the ion-exchange groups, the drug molecule is exchanged and diffuses out of the resins to the bulk solution. In this the rate limiting step is the surface area and the diffusion path length and further the release rate can be controlled by coating the drug-resin complex through microencapsulation and also by cross-linking.
3.3.2. pH-Independent Formulations
The drug administered orally encounters various spectrums of pH ranges in the GIT. As most of the drugs are weak acid or weak basis so their release from formulations are pH dependent thus could be controlled by adding buffers to the formulation. When gastric fluid enters the membrane, the buffer adjusts the polymer pH inside and imparts constant drug release.
3.3.3. Osmotically Controlled Release
Osmotic pressure provides constant drug release and acts as the driving force. When osmotic system is exposed to body fluid, it enters the core due to the osmotic pressure difference across the coating membrane. For this the drug must be osmotically active and is mixed with osmotically active excipients e.g., NaCl, KCl. Excipients helps to generate the osmotic pressure in the core, smaller the size of orifice more will be the hydrostatic pressure inside. For constant drug release equilibrium is maintained between hydrostatic and osmotic pressure. For further enhancement of permeation of GI fluids through the semi-permeable membrane, a bio-erodible polymer is coated on to the external surface.
3.3.4. Altered Density Formulations
The GI transit time varies from person to person; its range is 8-62 hrs. GI transit time gets affected by the physical properties of the delivery system and the presence of food. Multiple unit systems are less affected by the presence of food when compared to the single unit systems as they are uniformly distributed throughout the GI fluids. Density of delivery system must be in the range of 1-3 in order to have minimal influence by the GI transit time. Formulation density can be altered by following approaches:
3.3.4.1. High Density
Drug is mixed with heavy inert materials in order to have their density greater than that of the stomach content e.g., barium sulfates, titanium dioxide, iron powder and zinc oxide.
3.3.4.2. Low Density
The apparent density of pellets must be lower than that of gastric fluid. Sustained release is achieved by use of carriers such as polystyrol, poprice and popcorn. So the final product floats on the gastric fluids for prolonged time period. It has two modifications:
Modification -1
Buoyant tablet is modified as a bilayed tablet, one immediate release layer and other as sustained release layer.
Modification -2
By incorporation of a gas filled floatation chamber in to a micro porous drug reservoir compartment.
4. VARIOUS WORKS ON GASTRO-RETENTIVE DOSAGE FORM
Zhang C. et al., 2012 formulated Ofloxacin-loaded pellets by the extrusion-spheronization technique. Pellets were coated with three successive coatings-the retarding layer of ethyl cellulose, the effervescent layer of sodium bicarbonate and the polymeric layer of Eudragit® RL 30D that provides gas entrapment due to its swelling and water permeability properties. Pellets gave excellent floating and retarded drug release over 8 h studies [14]. Chaturvedi A.K. et al., 2011 prepared and evaluated floating microballoons of Norfloxacin by emulsion solvent diffusion method using Eudragit®L100 and Eudragit®RS100 in definite proportions. Eudragit®L100 dissolves above pH 6 whereas Eudragit®RS100 has pH independent dissolution. Gastric residence time was prolonged with an enhancement in bioavailability of drug. SEM study confirms their spherical shape with hollow cavity that provides buoyancy to the formulation [15]. Ehab H. et al., 2003 prepared and optimized Bumetanide extended as well as immediate release pellets. Pellets were formed by fluid bed layering and coating techniques. Coating dispersion comprises of 6% Eudragit®RS plasticized with 20% Tri ethyl citrate. Porosity of the pellets was increased by incorporating sodium chloride which acts as a channeling agent. Pellets gave faster dissolution and enhanced bioavailability [16]. Eytan K. et al., 2003 formulated novel unfolded controlled release-gastro retentive dosage form (CR-GRDF) for Levodopa by solvent evaporation method. The materials used were Gelatin, L-polylactic acid, ethyl cellulose, carbidopa Eudragit®S100, Shellac and microcrystalline cellulose. It was observed that the therapeutic concentration of the drug in plasma could be achieved over 9 h through the formulation design and confirmed by in vitro evaluation [17].
Atyabi F. et al., 1996 utilizes ion exchange resins as a novel floating effervescent system and evaluated in vivo for confirming the enhancement in residence time. Ion exchange resins are loaded with bi carbonate which when comes in contact with the acidic environment releases carbon dioxide causing the resin to float. These resins were further coated with Eudragit®RS for controlling the drug release and compared with the uncoated resins in vitro [18]. Jijun F. et al., 2011 formulated matrix controlled extended release pellets of Diclofenac potassium by extrusion-spheronization technique. The formed pellets were double layered using Eudragit®NE 30D, Eudragit®RS30D and Kollicoat®SR 30D coating polymers for better control of drug release and to avoid incomplete absorption of drug [19]. Di Colo G. et al., 2002 prepared and evaluated compressed matrix tablets of Metformin hydrochloride using polyethylene oxide and Eudragit®L100. The drug release could be modified by increasing the concentration of Eudragit®L100. The prepared matrices showed gradual and complete drug release without being fluctuated by the gastric pH [20]. Goole J, et al., 2008 formulated and evaluated floating coated mini-tabs of Levodopa for sustaining its release, the gas generating core containing drug was prepared by melt granulation followed by subsequent compression. The mini tabs formed were coated with Eudragit®RL 30D plasticized with acetyl tri ethyl citrate. Optimized formulation starts floating within 20 min and gave buoyancy over 13 h and sustained release over 20 h [21]. Kagan L. et al., 2006 formulated gastro retentive unfolding dosage form for Riboflavin for increasing its bioavailability without the need to be administered with high calorie meals. Coating polymers used were Eudragit®L and Eudragit®S plasticized with tri ethyl citrate. Results showed that Accordion pill technology was successful in prolonging the gastric residence time [22]. Ninan M. et al., 2008 prepared, optimized and evaluated effervescent floating microspheres of Diltiazem hydrochloride by Ionotropic gelation method using sodium alginate, calcium chloride, Eudragit®RS 30D and chitosan. Encapsulation was done by chitosan and the chitosan-alginate microspheres were further coated with Eudragit®RS30D to get prolonged gastro retentive time and a sustained release behavior. Calcium carbonate acts as a gas forming agent. Both coated and uncoated microspheres floated over 24 h in vitro. Floating microsphere stayed over 5 h whereas non- floating was emptied with in 2.5 h [23].
Patel S.R. et al., 2010 formulated and optimized enteric coated tablets of Rabeprazole sodium employing colorcoat®EC4S, Mannitol SD200, microcrystalline cellulose and kollidon®CL by wet granulation and direct compression method. The formulation showed resistance in acidic environment and sustained its release in alkaline environment. Colorcoat®EC4S retards the release pattern of the drug thereby enhancing the therapeutic efficacy [24]. Strubing S. et al., 2008 formulated sustained release matrix tablet of Propanolol hydrochloride using Kollidon®SR by direct compression method. The release kinetic showed korsmeyer peppas model following fickian diffusion. Kollidon®SR sustained the release over a period of 24 h with fickian diffusion kinetics [25]. Sato Y. et al., 2003 prepared and in vivo evaluated the sustained release action of the prepared microballoons containing Riboflavin as the model drug by emulsion solvent diffusion method. Eudragit®RS100 and hydroxyl propyl methyl cellulose in different ratios were dissolved in ethanol and dichloro methane. Study was carried out in healthy volunteers and the result showed that the urinary excretion of the drug was sustained with the increase in overall urinary excretion [26]. El-Kamel A.H. et al., 2001 develpoed floating microparticles of Ketoprofen using different ratios of Eudragit®S100 and Eudragit®RL100 by emulsion solvent diffusion method. They observed that the drug content of the prepared microparticles decreases with increase in concentration of Eudragit®RL100 whereas similar concentration of both gave higher percentage yield and better buoyancy [27]. Sato Y. et al., 2004 formulated and evaluated Riboflavin microballoons using Eudragit®S100, HPMC, PVA, dichloro methane and ethanol by emulsion solvent diffusion method. They found that by varying the concentration of HPMC release profiles could be improved. The statistical evaluation confirms the correlation between buoyancy and excretion half life and between drug release and total urinary excretion [28]. Sawicki W., 2002 studied Pharmacokinetics of verapamil in a dose of 40 mg and its metabolite nor-verapamil from the new oral drug formulation in a form of capsule filled with floating pellets was determined. Pellets were prepared by wet granulation and spheronization technique. Core of the pellets contains the drug, microcrystalline cellulose, lactose and povidone K 30 whereas thick film coat contains Eudragit®NE 30D, Eudragit®L30D, triethyl citrate and talcum. Floating drug formulation is a gelatin capsule filled with pellets with verapamil in a dose of 40 mg, coated with a control release film. Capsule filled with floating pellets floated for 6 h and gave better pharmacokinetic results in comparison to the conventional tablets [29]. Sato Y. et al., 2003 developed hollow and buoyant microballoons of Aspirin, Salicylic acid, Ethoxybenzamide, Riboflavin and Indomethacin employing emulsion solvent diffusion method. A mixture of drug, Eudragit®S100 and monostearin were dissolved in dichloro methane and ethanol mixture and poured slowly in to the poly vinyl alcohol solution kept at 40oC with constant stirring speed and stirred continuously for 1h. The in vitro release behaviors of different drugs were studied and it was found that the buoyancy of microballoons decreases with increase release behavior. Optimum temperature of 40 oC gave better buoyancy and retarded release was due to smooth surface. Drug entrapment was high due to higher distribution coefficient [30]. Sato Y. et al., 2004 developed floating as well as non-floating microballoons of Riboflavin for investigating their gastro retentive time in the stomach. Floating microballoons were prepared by using Eudragit®RS100 and HPMC in different ratios by emulsion solvent diffusion method. The intra gastric behavior of the dosage form showed similar release profiles when investigated through gamma scintigraphy technique in both fasted and the fed conditions. The study confirms that the floating microballoons retained for longer time period in comparison to the non-floating in fed conditions, both half life and the total urinary excretion of drug increases significantly due to prolonged retention of the dosage form in the gastric fluids [31].
Tao S.L. et al., 2003 developed bio-adhesive devices by microfabrication technology for the oral delivery of proteins and peptides by protecting from gastrointestinal denaturation, localizing and prolonging at a specific target site and to maintain direct contact with the intestinal cells in order to increase the drug concentration gradient. Lectins, a group of proteins capable of targetting to the intestinal cells imparts bio-adhesive properties on attachment with the microfabricated poly (methyl methacrylate) (PMMA) micro devices. Avidin molecules covalently bind with the amine groups of PMMA. The in vitro analysis showed prevention of drug denaturation and prolongs the release rate [32] (Table 1).
5. CHEMICAL COMPOSITIONS
- Poly [Butyl methacrylate, (2-dimethylaminoethyl) methacrylate, methyl methacrylate] with the ratio 1:2:1, trade names Eudragit®E100, Eudragit®E12.5 and Eudragit®EPO are manufactured and marketed by Evonik Industries (Fig. (2a)).
- Poly [Ethyl acrylate, methyl methacrylate] with the ratio 2:1, trade names Eudragit®NE30D, Eudragit®NE40D and Eudragit®NM30D are manufactured and marketed by Evonik Industries (Fig. (2b)).
- Poly [methacrylic acid, methyl methacrylate] with the ratio 1:1, trade names Eudragit®L100, Eudragit®L12.5 and Eudragit®L12.5P are manufactured and marketed by Evonik Industries (Fig. (2c)).
- Poly [methacrylic acid, ethyl acrylate] with the ratio 1:1, trade names Acryl-EZE, Acryl-EZE 93A and Acryl-EZE MP are manufactured and marketed by Colorcon. Trade names Eudragit®L 30 D-55 and Eudragit®L 100-55 by Evonik Industries, trade name Eastacryl®30 D by Eastman Chemical and with trade names Kollicoat®MAE 30 DP and Kollicoat®MAE 100 P by BASF Fine Chemicals (Fig. (2d)).
- Poly [methacrylic acid, methyl methacrylate] with the ratio 1:2, trade names Eudragit®S100, Eudragit®S12.5 and Eudragit®S12.5P are manufactured and marketed by Evonik Industries (Fig. (2e)).
- Poly [Methyl acrylate, methyl methacrylate, methacrylic acid] with the ratio 7:3:1, trade name Eudragit®FS 30D are manufactured and marketed by Evonik Industries (Fig. (2f)).
- Poly [Ethyl acrylate, methyl methacrylate, trimethylammonioethyl methacrylate chloride] with the ratio 1:2:0.2, trade names Eudragit®RL100, Eudragit®RLPO, Eudragit®RL 30D and Eudragit®RL 12.5 are manufactured and marketed by Evonik Industries (Fig. (2g)).
- Poly [Ethyl acrylate, methyl methacrylate, trimethylammonioethyl methacrylate chloride] with the ratio 1:2:0.1, trade names Eudragit®RS100, Eudragit®RSPO, Eudragit®RS 30D and Eudragit®RS 12.5 are manufactured and marketed by Evonik Industries, (Fig. (2h)) [33](Table 2).
6. PHARMACEUTICAL APPLICATIONS AND DESCRIPTION
They are primarily used as film forming agent, tablet binders and tablet diluents etc. (Table 3). Eudragit®E12.5 is available as organic solution, as a 12.5 % solution in propanol-acetone (60:40). It is light yellowish in color, soluble in gastric pH below 5, used as a film coating agent. It is miscible in acetone-alcohols, dichloromethane, ethyl acetate, 1N HCl and petroleum ether. Eudragit®E100 targeted area is stomach and it consists of colorless to yellow tinged granules with a characteristic amine-like odor. It has low viscosity, high pigment binding capacity, good adhesion and low polymer weight gain. It is soluble in gastric pH below 5 and solvents like acetone-alcohols, dichloromethane and ethyl acetate. Eudragit®E PO is available as white free-flowing powder forms 98 % ready to use solutions in acetone and alcohols. Both are soluble in gastric pH below 5 and used as a film coating material.
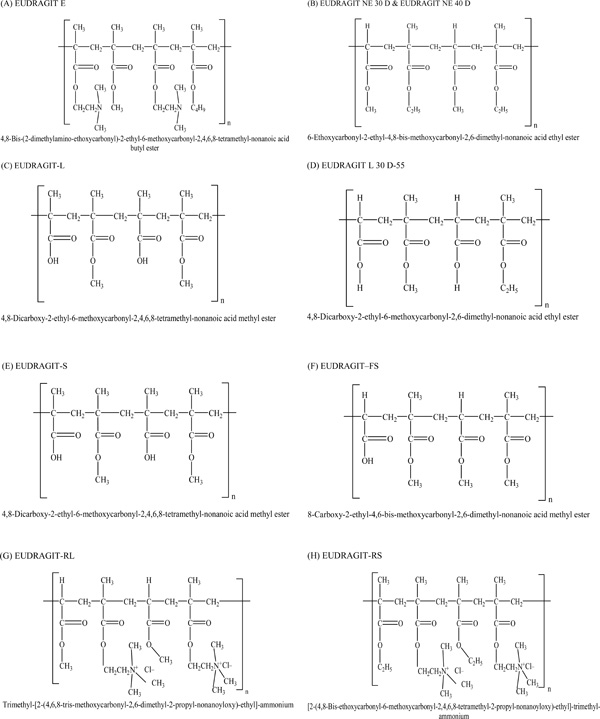 |
Fig. (2). Chemical structures and IUPAC names of polymethacrylates. |
Chemical name, trade name and company name of Polymethacrylates.
| S. No. | Chemical name | Polymer Ratio | Trade name | Company name | Company address |
|---|---|---|---|---|---|
| 1. | Poly[Butyl methacrylate, (2-dimethylaminoethyl) methacrylate, methyl methacrylate] | 1:2:1 | Eudragit® E 100 Eudragit® E 12.5 Eudragit® E PO | Evonik Industries | Essen, Germany |
| 2. | Poly[Ethyl acrylate, methyl methacrylate] | 2:1 | Eudragit® NE 30 D Eudragit® NE 40 D Eudragit® NM 30 D | Evonik Industries | Essen, Germany |
| 3. | Poly[methacrylic acid, methyl methacrylate] | 1:1 | Eudragit® L 100 Eudragit® L 12.5 Eudragit® L 12.5 P | Evonik Industries | Essen, Germany |
| 4. | Poly[methacrylic acid, ethyl acrylate] | 1:1 | Acryl-EZE | Colorcon | Pennsylvania, U.S. |
| Acryl-EZE 93A | Colorcon | Pennsylvania, U.S. | |||
| Acryl-EZE MP | Colorcon | Pennsylvania, U.S. | |||
| Eudragit® L 30 D-55 | Evonik Industries | Essen, Germany | |||
| Eudragit® L 100-55 | Evonik Industries | Essen, Germany | |||
| Eastacryl 30 D | Eastman Chemical | Kingsport, Tennessee, U.S. | |||
| Kollicoat® MAE 30 DP | BASF Fine Chemicals | Ludwigshafen, Germany | |||
| Kollicoat® MAE 100 P | BASF Fine Chemicals | Ludwigshafen, Germany | |||
| 5. | Poly[methacrylic acid, methyl methacrylate] | 1:2 | Eudragit® S 100 Eudragit® S 12.5 Eudragit® S 12.5 P | Evonik Industries | Essen, Germany |
| 6. | Poly[Methyl acrylate, methyl methacrylate, methacrylic acid] | 7:3:1 | Eudragit® FS 30 D | Evonik Industries | Essen, Germany |
| 7. | Poly[Ethyl acrylate, methyl methacrylate, trimethylammonioethyl methacrylate chloride] | 1:2:0.2 | Eudragit® RL 100 Eudragit® RL PO Eudragit®RL 30 D Eudragit® RL 12.5 | Evonik Industries | Essen, Germany |
| 8. | Poly[Ethyl acrylate, methyl methacrylate, trimethylammonioethyl methacrylate chloride] | 1:2:0.1 | Eudragit® RS 100 Eudragit® RS PO Eudragit® RS 30 D Eudragit® RS 12.5 | Evonik Industries | Essen, Germany |
Eudragit®L 12.5P and Eudragit®L 12.5 supplied as organic solution, as a 12.5 % ready to use solution in acetone and alcohols, used as an enteric coating agent. Their film coats are resistant to gastric media but soluble in intestinal fluids above pH 6 and shows miscibility in acetone-alcohols, dichloromethane, ethyl acetate and 1N NaOH. Eudragit®L100 is a solid substance in form of a white powder with a faint characteristic odor, ready to use as a 95 % solution in acetone and alcohols and also shows solubility in 1N NaOH, used as an enteric coating agent with solubility in intestinal fluids above pH 6. Its targeted drug release area is jejunum. It has effective and stable enteric coatings with a fast dissolution in the upper bowel. It does granulation of drug substances in powder form for controlled release. It also shows variable release profiles and site specific drug delivery in intestine in combination with Eudragit®S grades. Eudragit®L 100-55 is also available as a powder with 95 % ready to use solution in acetone and alcohols and shows solubility in 1N NaOH. Soluble in intestinal fluids above pH 5.5, used to form enteric coat films. Eudragit®L30 D-55 is supplied as aqueous dispersion with 30 % solution in water having solubility in intestinal fluids above pH 5.5, used to make enteric coats. It shows miscibility in acetone-alcohols, 1N HCl and petroleum ether. Eudragit®S 12.5P and Eudragit®S 12.5 are supplied as organic solution with 12.5 % ready to use solution in acetone and alcohols. It is soluble in intestinal fluid above pH 7 and used as an enteric coating polymer. They show miscibility in acetone-alcohols, dichloromethane, ethyl acetate and 1N NaOH. Eudragit®S100 is soluble in intestinal fluid above pH 7, soluble in solvents like acetone-alcohols and 1N NaOH. Available in the form of powder and its targeted drug release area is colon. It does granulation of drug substances for controlled release, effective and stable enteric coatings with a fast dissolution in the upper bowel. It shows variable release profiles with site specific drug delivery in intestine in combination with Eudragit®S grades [33].
Eudragit®FS 30D is supplied in aqueous dispersion form with 30 % ready to use dispersion in water. It is used as an enteric coating polymer with dissolution in intestinal fluid above pH 7. The ammonium groups in Eudragit®RL and RS provides pH-independent permeability to the polymers. Both polymers are water-insoluble. Eudragit®RL films are freely permeable to water and other dissolved active substances, while films prepared from Eudragit®RS are only slightly permeable to water. Eudragit®RL100 and RS 100 are granular in form with a low content of quaternary ammonium groups [3]. Eudragit®RL 12.5, Eudragit®RL 100, Eudragit®RL PO and Eudragit®RL 30 D shows high permeability and sustained release profiles. Eudragit®RL 12.5 is available as organic solution with 12.5 % solution in acetone and alcohols, miscibility in dichloromethane, ethyl acetate and water. Eudragit®RL100 is a solid substance in form of colorless, clear to cloudy granules with a faint amine like odor and forms 97 % solution in acetone and alcohols and also shows solubility in solvents like dichloromethane and ethyl acetate. Eudragit®RL PO is a solid substance in form of white powder with a faint amine-like odor with 97 % solution in acetone and alcohols, solvents like dichloromethane and ethyl acetate and Eudragit®RL 30D is a milky-white liquid of low viscosity with a faint characteristic odor. Eudragit®RL 30D as aqueous dispersion with 30 % ready to use in water and miscibility in solvents like acetone and alcohols, dichloromethane, ethyl acetate and water.
Properties and uses of commercially available polymethacrylates.
| S.No. | Grade® | Supply form | Polymer dry weight content (% w/w) | Recommended solvents or diluents | Solubility/Permeability | Applications |
|---|---|---|---|---|---|---|
| 1. | Eudragit E 12.5 | Organic solution | 12.5% | Acetone, Alcohols | Solution in gastric fluid to pH 5 | Film coating |
| 2. | Eudragit E 100 | Granules | 98% | Acetone, Alcohols | Solution in gastric fluid to pH 5 | Film coating |
| 3. | Eudragit E PO | Powder | 98% | Acetone, Alcohols | Solution in gastric fluid to pH 5 | Film coating |
| 4. | Eudragit L 12.5 P | Organic solution | 12.5% | Acetone, Alcohols | Solution in intestinal fluid from pH 6 | Enteric coatings |
| 5. | Eudragit L 12.5 | Organic solution | 12.5% | Acetone, Alcohols | Solution in intestinal fluid from pH 6 | Enteric coatings |
| 6. | Eudragit L 100 | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 6 | Enteric coatings |
| 7. | Eudragit L 100-55 | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 8. | Eudragit L 30 D-55 | Aqueous dispersion | 30% | Water | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 9. | Eudragit S 12.5 P | Organic solution | 12.5% | Acetone, Alcohols | Solution in intestinal fluid from pH 7 | Enteric coatings |
| 10. | Eudragit S 12.5 | Organic solution | 12.5% | Acetone, Alcohols | Solution in intestinal fluid from pH 7 | Enteric coatings |
| 11. | Eudragit S 100 | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 7 | Enteric coatings |
| 12. | Eudragit FS 30 D | Aqueous dispersion | 30% | Water | Solution in intestinal fluid from pH 7 | Enteric coatings |
| 13. | Eudragit RL 12.5 | Organic solution | 12.5% | Acetone, Alcohols | High permeability | Sustained release |
| 14. | Eudragit RL 100 | Granules | 97% | Acetone, Alcohols | High permeability | Sustained release |
| 15. | Eudragit RL PO | Powder | 97% | Acetone, Alcohols | High permeability | Sustained release |
| 16. | Eudragit RL 30 D | Aqueous dispersion | 30% | Water | High permeability | Sustained release |
| 17. | Eudragit RS 12.5 | Organic solution | 12.5% | Acetone, Alcohols | Low permeability | Sustained release |
| 18. | Eudragit RS 100 | Granules | 97% | Acetone, Alcohols | Low permeability | Sustained release |
| 19. | Eudragit RS PO | Powder | 97% | Acetone, Alcohols | Low permeability | Sustained release |
| 20. | Eudragit RS 30 D | Aqueous dispersion | 30% | Water | Low permeability | Sustained release |
| 21. | Eudragit NE 30 D | Aqueous dispersion | 30% | Water | Swellable, permeable | Sustained release, tablet matrix |
| 22. | Eudragit NE 40 D | Aqueous dispersion | 40% | Water | Swellable, permeable | Sustained release, tablet matrix |
| 23. | Eudragit NM 30 D | Aqueous dispersion | 30% | Water | Swellable, permeable | Sustained release, tablet matrix |
| 24. | Eastacryl 30 D | Aqueous dispersion | 30% | Water | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 25. | Kollicoat MAE 30 DP | Aqueous dispersion | 30% | Water | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 26. | Kollicoat MAE 100 P | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 27. | Acryl-EZE | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 28. | Acryl-EZE 93 A | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
| 29. | Acryl-EZE MP | Powder | 95% | Acetone, Alcohols | Solution in intestinal fluid from pH 5.5 | Enteric coatings |
Eudragit®RS 12.5, Eudragit®RS 100, Eudragit®RS PO and Eudragit®RS 30 D shows low permeability and sustained release profiles. Eudragit®RS 12.5 is available as organic solution with 12.5 % solution in acetone and alcohols and shows miscibility in dichloromethane, ethyl acetate and water. Eudragit®RS100 is a solid substance in form of colorless, clear to cloudy granules with a faint amine-like odor and forms 97 % solution in acetone and alcohols and also soluble in solvents like dichloromethane and ethyl acetate. The ammonium groups are present as salts and make the polymers permeable.Eudragit®RS PO is available as powder with 97 % solution in acetone and alcohols and soluble in solvents like dichloromethane and ethyl acetate. Eudragit®RS 30D as aqueous dispersion with 30 % ready to use in water and solvents like acetone and alcohols, dichloromethane, ethyl acetate and water.
Eudragit®NE 30D and Eudragit®NE 40D are available as 30 % and 40 % aqueous dispersion in water. Both shows swellable and permeable behavior and are used as sustained release polymers in tablet matrix. The dispersions are milky-white liquids of low viscosity and have a weak aromatic odor. So the films produced are insoluble in water, but gives pH-independent drug release. Eudragit®NM 30D is of identical monomer composition to Eudragit®NE 30D. It shows swellable and permeable behavior and is used as sustained release polymer in tablet matrix.
In Eastacryl®30D and Kollicoat®MAE 30DP the ratio of free-carboxyl groups to ester groups is 1:1. Films formed dissolves above pH 5.5; forming salts with alkali, thus film formed are insoluble in gastric media but soluble in the small intestine. They both show miscibility in acetone and alcohols, 1N NaOH and water. Acryl-EZE, Acryl-EZE 93 A and Acryl-EZE MP are commercially available as redispersible powder forms, which are used as enteric coat polymers in case of tablets and beads and are solubilized in intestinal fluid above pH 5.5. They are soluble in solvents acetone and alcohols and 1N NaOH.
7. GLASS TRANSITION TEMPERATURE (Tg)
In the description of physical properties of polymers Tg plays an important role (Table 4). On a macroscopic level it describes the solidification of an anisotropic polymer melt. The Tg has far-reaching consequences, e.g., for film formation, melt processing and storage of finished pharmaceutical dosage forms. Plasticizers, solvents or residual solvents (including water) that act as plasticizers usually cause a reduction in Tg, which is specifically exploited in application formulations. Most common plasticizer for Eudragit® polymers is tri ethyl citrate (TEC).
Glass transition temperatures (Tg) of different Eu-dragit grades.
| S. No. | Eudragit® grade | Tg (ºC) |
|---|---|---|
| 1. | Eudragit E 100 / E PO | 48 |
| 2. | Eudragit E 12.5/ 12.5 P | 45 |
| 3. | Eudragit L 100 | Greater than 130 |
| 4. | Eudragit L 100-55 / L 30 D-55 | 110 |
| 5. | Eudragit L 12.5 | 130 (± 5) |
| 6. | Eudragit S 100 | 130 (± 5) |
| 7. | Eudragit S 12.5/ 12.5 P | 130 (± 5) |
| 8. | Eudragit FS 30 D | 48 |
| 9. | Eudragit RL 100 / RL PO | 63 |
| 10. | Eudragit RL 30 D/ RS 30 D | 55 |
| 11. | Eudragit RS 100 / RS PO | 65 |
| 12. | Eudragit NE 30 D/ 40 D | -8 |
| 13. | Eudragit NM 30 D | 11 |
Physical properties of polymers in film coating formulations could be modified by the addition of plasticizers as it decreases the film brittleness. It is generally accepted that the mechanism by which polymers exerts their action is for them to interpose themselves on a molecular scale between the polymer strands. In doing so they permit these strands to move more freely and allow the polymer to act in a more pliable fashion [34].
In order to enhance the solubility of polymers various plasticizers are recommended in the concentration 10-25%, they are dibutyl phthalate (DBT), polyethylene glycols (PEG), TEC, tri acetin, and 1, 2-propylene glycol. Plasticizers are not required in Eudragit®E12.5, Eudragit®E100 and Eudragit®NE 30D. The Tg could be lowered by adding small amounts of plasticizers that fits between the glassy molecules, gives them mobility and thus increases the solubility. The Tg of Eudragit®RL and RS polymers are as high as 70°C and 65°C respectively. While the minimum film formation temperature (MFT) of the aqueous dispersions Eudragit®RL 30D and RS 30D are 40°C and 45°C respectively [6]. These polymers require the addition of a plasticizer, usually in the range of 5 % to 30 %, calculated on dry polymer mass, to reduce the MFT of aqueous dispersion in order to ensure proper film formation and improve film properties [35].
CONCLUSION
Different grades of polymethacrylates are commercially available to achieve the pH dependent drug release for enhancing the bioavailability and minimizing the side effects. They are applied as film coat, enteric coat, sustaining the drug release and as a tablet matrix. Tg of polymers helps in enhancing their solubility by use of suitable plasticizers. While designing the dosage forms one should have the complete knowledge of the polymer behavior, the pharmacokinetics of the drug and their toxicological effects. This review may be helpful in polymer selection for the site specific delivery. The contributions given by researchers on Eudragit® polymers applications showed their future potential and significance.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We the authors wish to express our gratitude to Sir Madanlal Institute of Pharmacy, Etawah (U.P), India and Rajiv Academy of Pharmacy, Mathura (U.P), India for their assistance, guidance and motivation in literature survey and manuscript preparation.